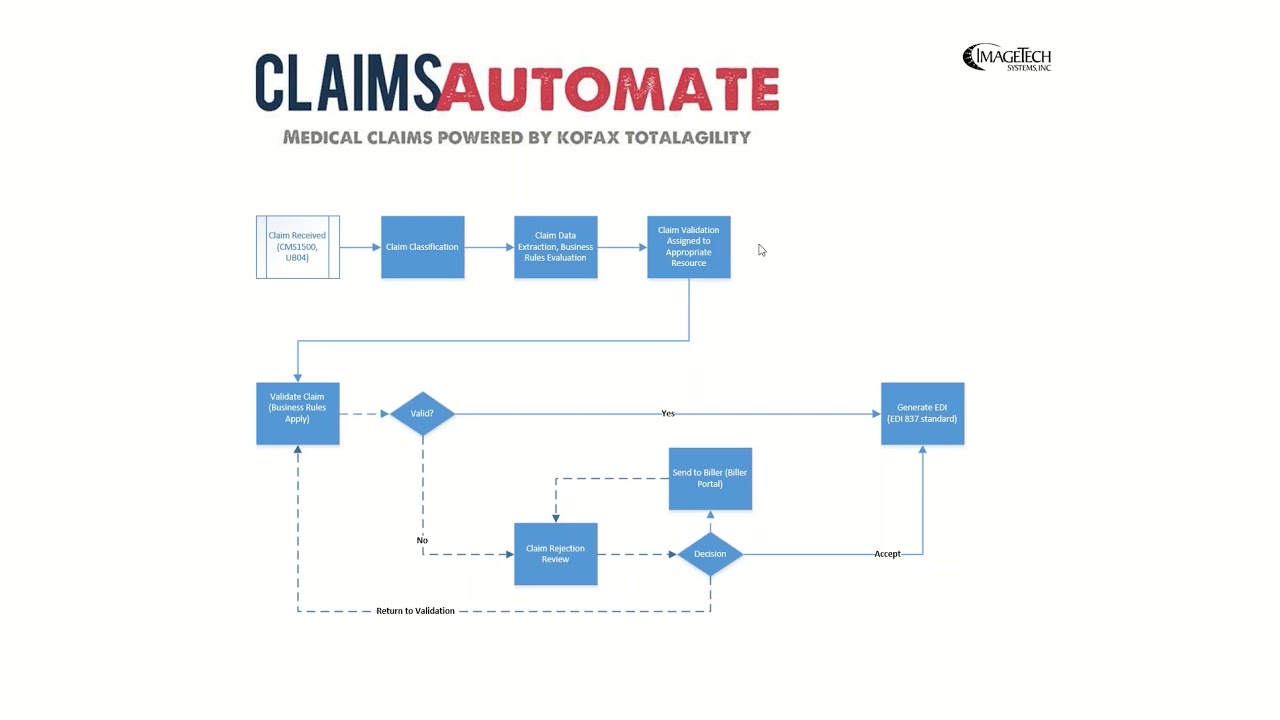
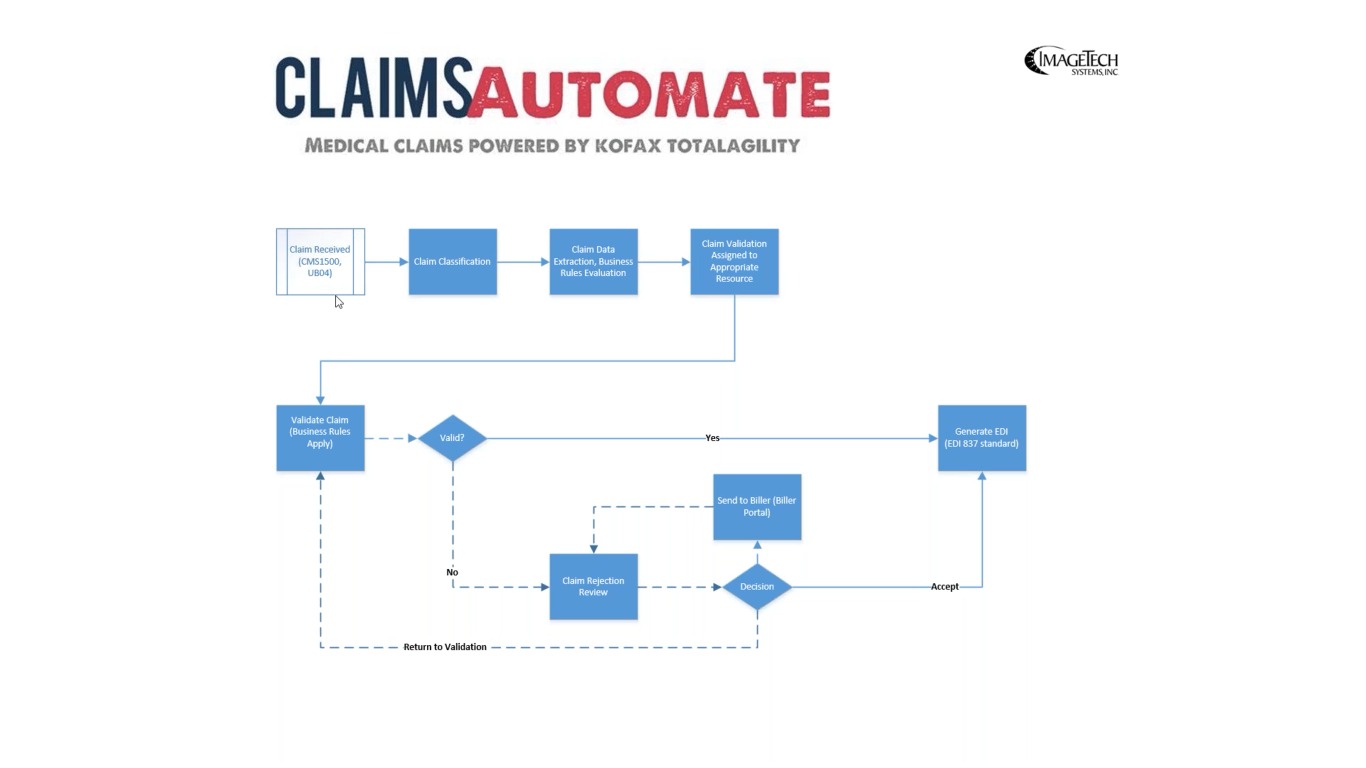
CLAIMSAutomate Medical Claims Processing for TotalAgility
CLAIMSAutomate Medical Claims Processing for TotalAgility Overview
Features
- Automatic classification of professional and institutional claims
- Support for multi-channel capture and rejection workflows
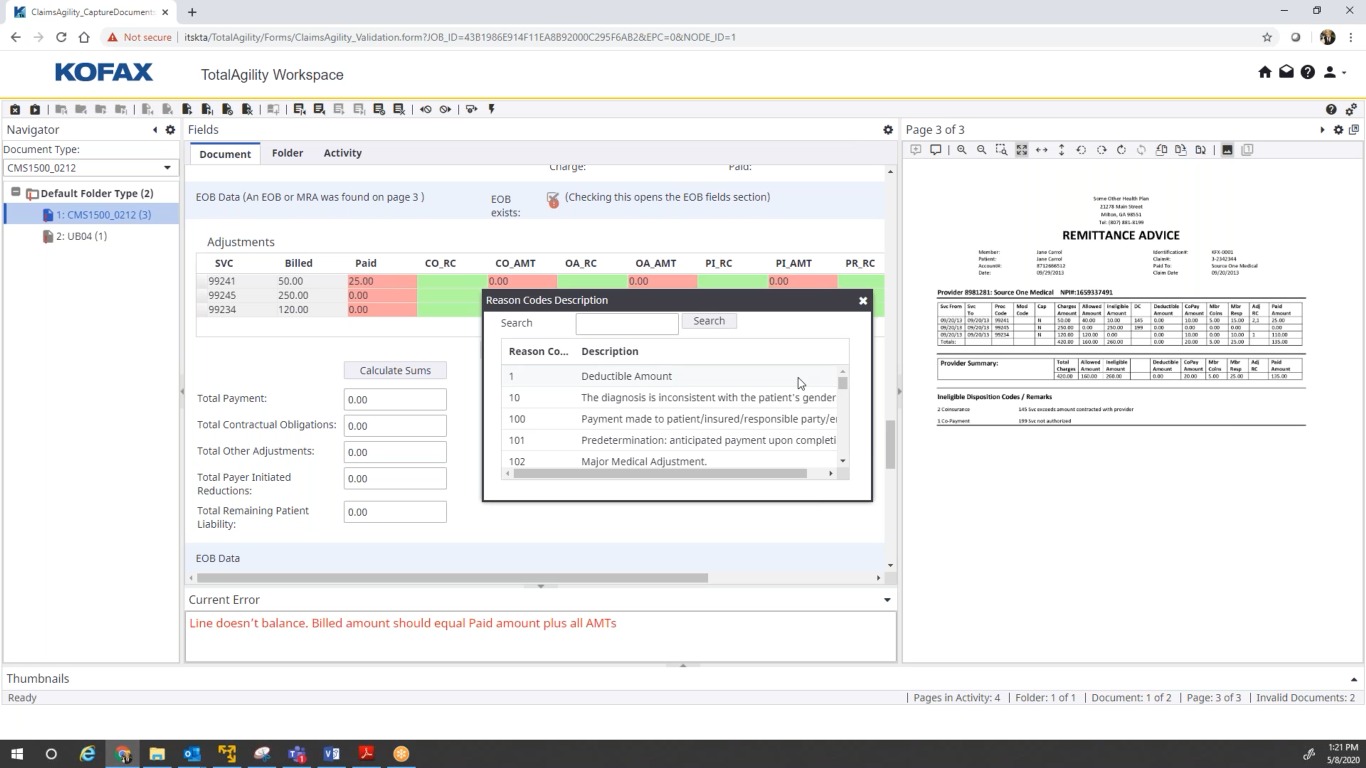
- 100s of pre-built business rules to enforce the specifications that govern the medical forms and EDI
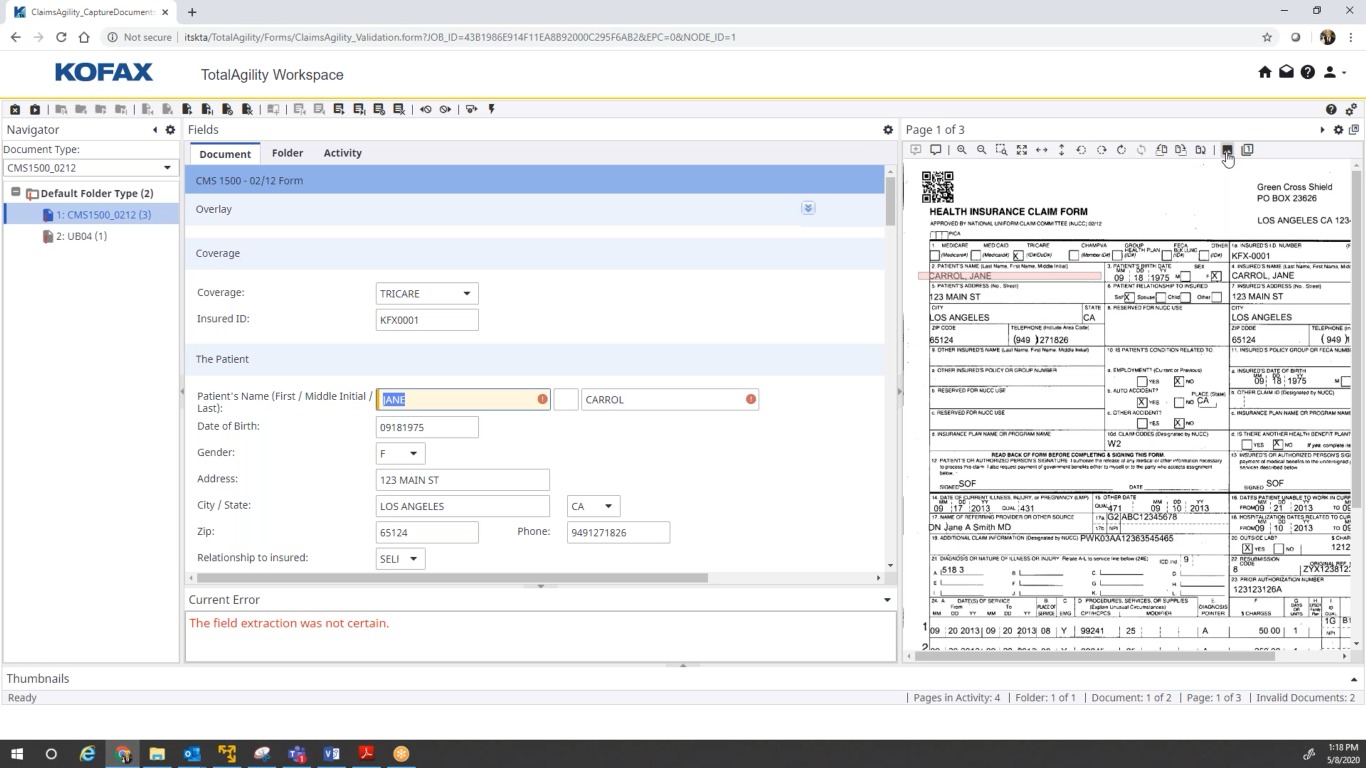
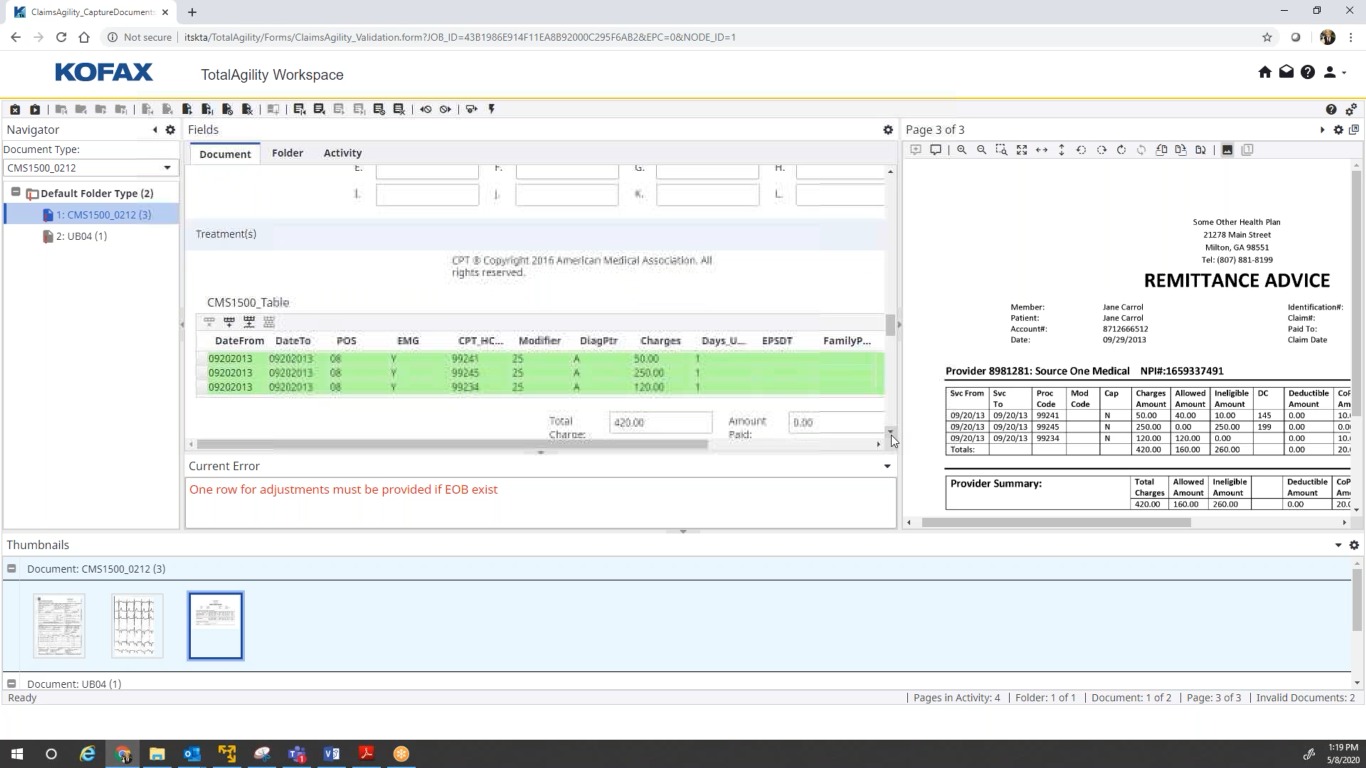
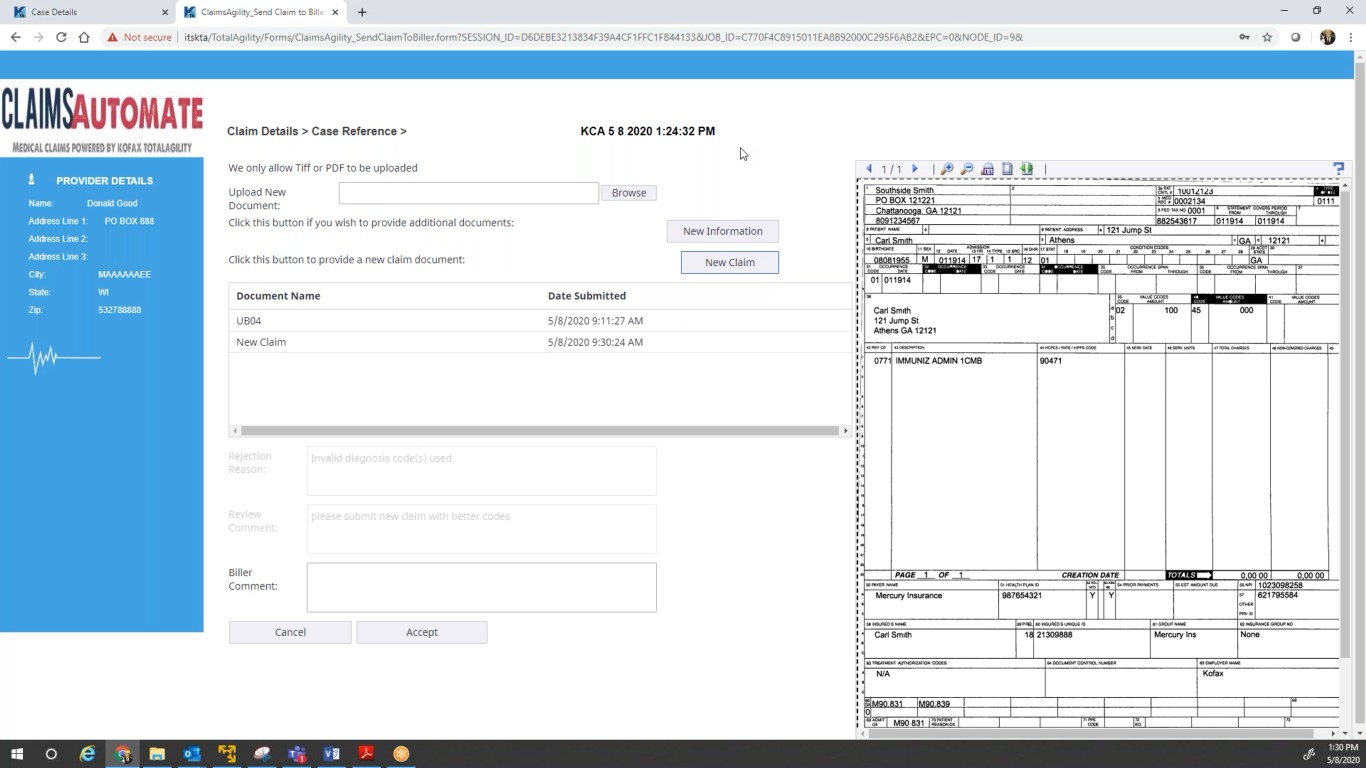
- A validation operator UI to review, correct and disposition claims, and to capture EOBs/Remittance Advice
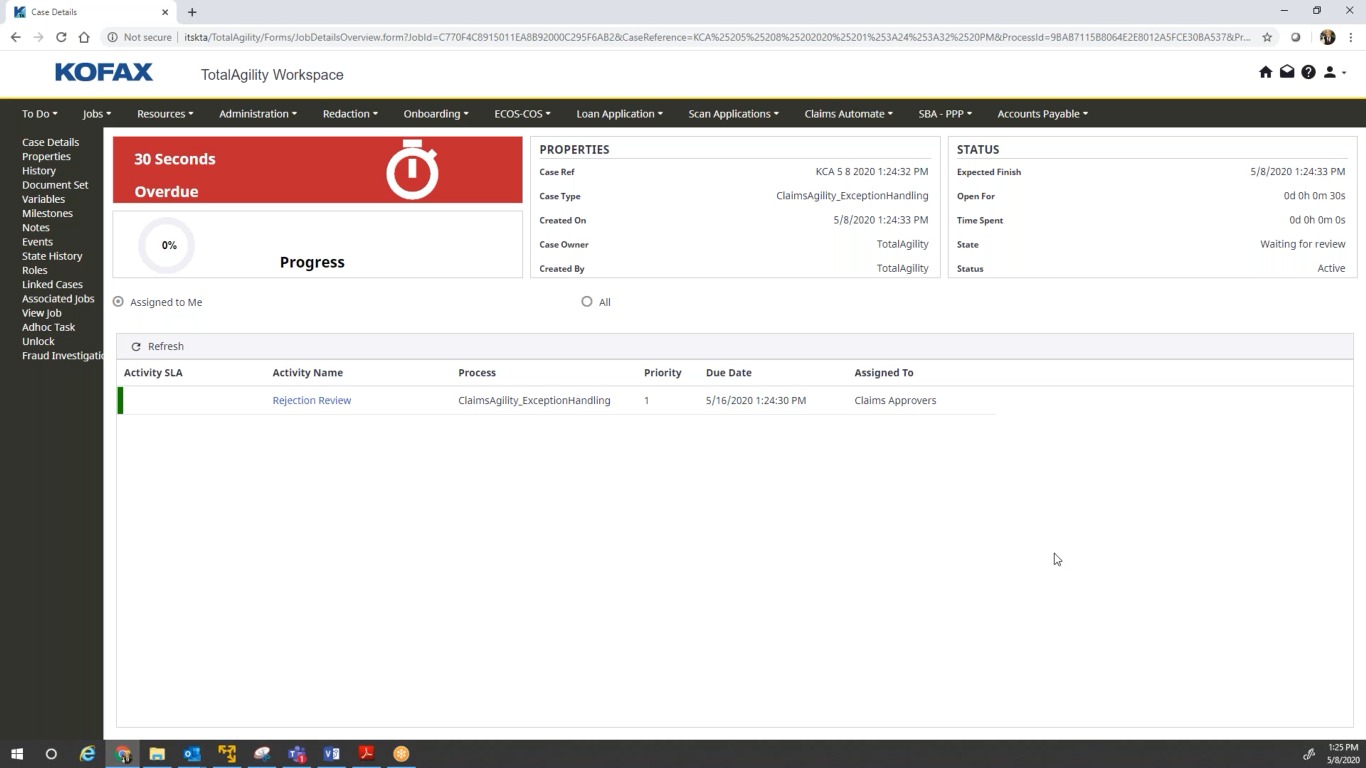
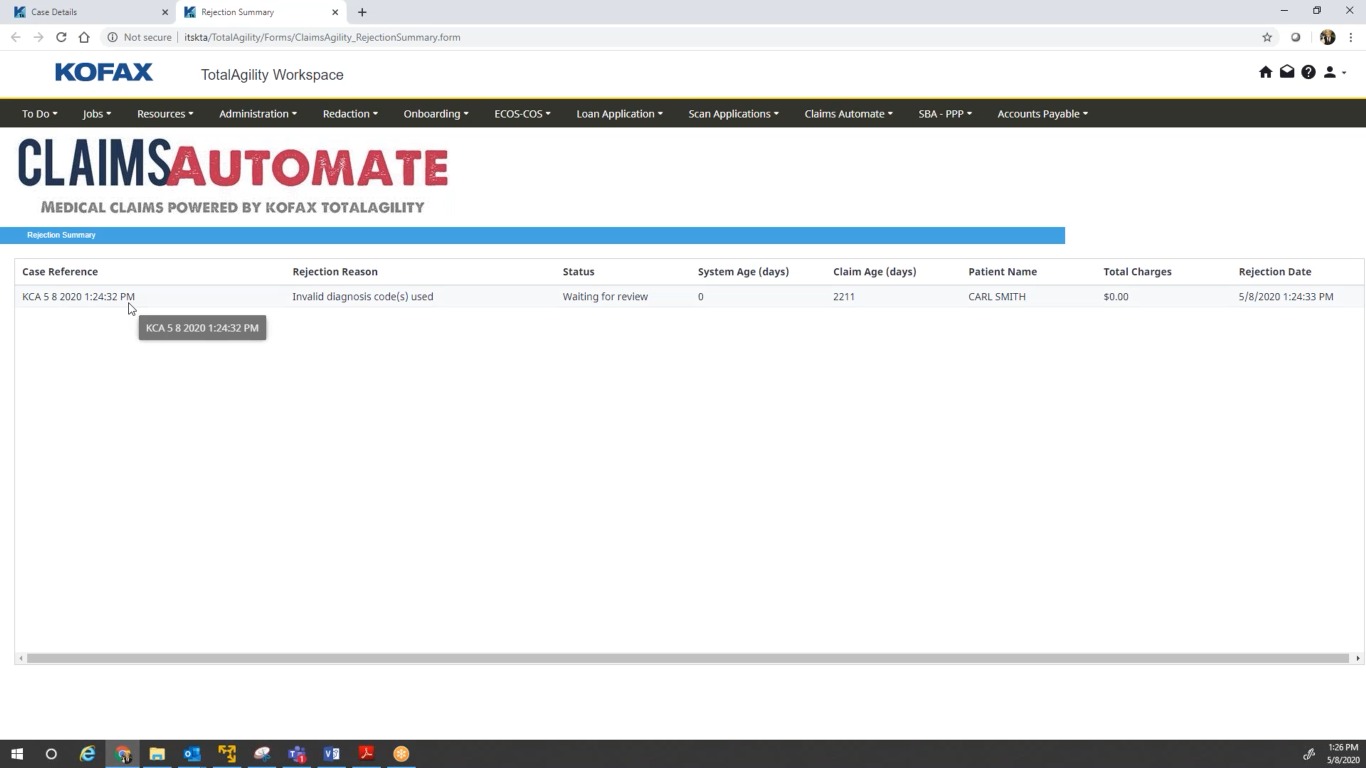
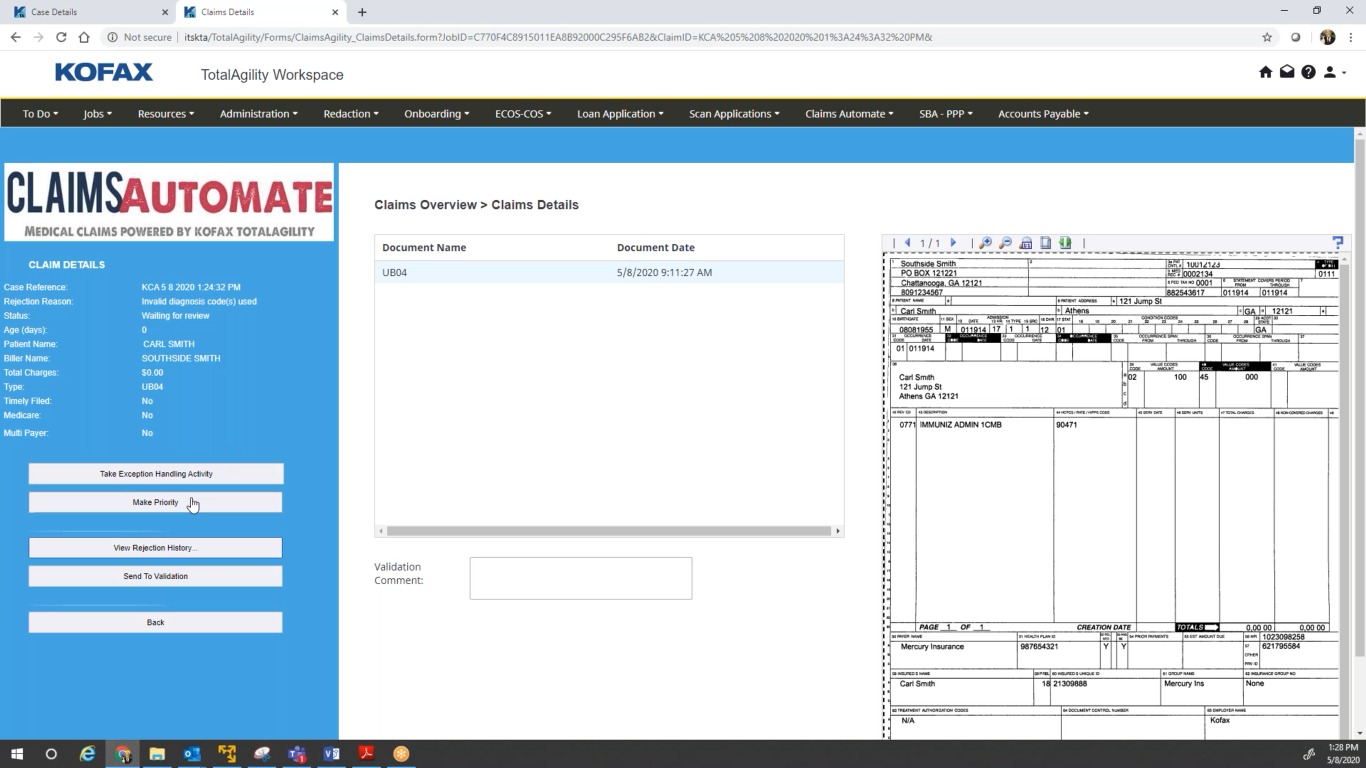
- An examiner user interface to review and manage rejections and communicate with providers to resolve problematic claims through a 24x7 web portal
- An exception handling framework for routing claims automatically into exception workflows
- Automatic export of clean claims to an ANSI X12-compliant EDI format (837 v5010) for handoff to the downstream adjudication process
- Integration with Kofax Analytics for monitoring capture analytics and processing paths for identifying bottlenecks and making informed process improvements
Benefits
- Reduced Manual Paper Handling
- Automated Extraction of Key Medical Data
- Fewer Lost & Duplicate Bills or Supporting Documents
- Increased Visibility of Claims Status
- Workflows that Manage Exceptions
- Stronger Internal Controls
- Integration to Adjudication & LOB Systems
- Decreased HIPAA Risk Due to Unprotected PHI
Technical Details
Inputs
ClaimsAutomate can be configured to process CMS-1500 and UB-O4 claim forms, as well as all supporting documentation, EOB (Explanation of Benefits) forms, Remittance Advice, and more.
Outputs
ClaimsAutomate can export EDI, XML, CSV, and other common formats.